Compassion & Choices is working to raise awareness about and the availability of hospice care, as well as fully empower all communities to access available care and to improve access to hospice care, especially for historically underserved communities, through federal policy change.
What Is Hospice?
Hospice provides comprehensive, holistic support for terminally ill people and those close to them including comfort care and the relief of physical, psychological and spiritual suffering.
Why Does Compassion & Choices Support Public Education and Policy Solutions to Improve Access to Hospice Care?
Hospice care directly aligns with our mission of improving care and empowering everybody to chart their own end-of-life journey. Through hospice care, patients with advanced illness who are nearing the end of life have access to care that is focused on improving quality of life and improving the dying process.
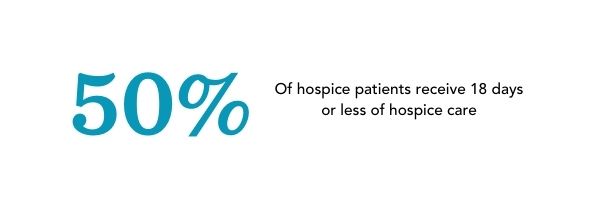
Too many people are unaware of the benefits of hospice care or are not provided with a timely referral. As a result patients, especially historically underserved patients, only benefit from hospice care for a very short period of time.
Unfortunately, while hospice is available to patients with a terminal prognosis of six months or less, the vast majority of people are enrolled in hospice for far less than six months. According to the National Hospice and Palliative Care Organization’s Facts and Figures, the average length of stay for Medicare patients enrolled in hospice in 2019 was 92.6 days. The median length of stay was 18 days.
.png?sfvrsn=9ede0fe2_3)
What Does Hospice Provide?
Hospice programs provide integrated services to manage a patient’s terminal illness with a focus on achieving the best quality of life through aggressive symptom management aimed at relieving pain and suffering. The patient and family together are considered the client as both receive services. Services vary by hospice, however. Core services include:
- The development of an individualized care plan designed to address the physical, emotional and spiritual needs that often accompany terminal illness.
- Routine care in a patient’s home, an assisted living facility, nursing home or Skilled Nursing Facility (SNF) with service levels varying depending on the disease progression.
- Respite care for the express purpose of giving the primary caregiver (usually the family) a break or to allow them to attend to family business.
- Short-term inpatient care for symptom control associated with the patient’s terminal illness that cannot be managed in the home setting.
- Continuous care in the home, at an assisted living facility, or at a contracted nursing home or a contracted SNF for as much as 24 hours a day during periods of medical crisis or to manage medical symptoms associated with the patient's terminal illness.
- Counseling services including, spiritual care psychological service and bereavement support after death.
- Medical supplies, durable medical equipment, and medications associated with the terminal diagnosis.
- Planning support for funeral arrangements and disposition.
Beyond the core services, some hospices provide other services, such as:
- Complementary medicine: including music therapy, art therapy, massage, acupuncture, etc.
- Occupational therapy
- Speech language pathology
- Physical Therapy
If any of these services are important to you, check with your hospice while interviewing to confirm whether they are offered.
Is Hospice Covered by Insurance?
Hospice is covered by Medicare Part A, Medicaid and most private insurance plans. If the patient has Medicare and meets hospice eligibility requirements, then typically 100% of the cost of hospice care is paid for with no deductible and no copayment for the patient. Medicaid also provides coverage, but that varies by state.
Nine out of 10 hospice patients rely on Medicare and Medicaid to cover their care. The remaining patients who are not on either Medicare or Medicaid can typically receive hospice through private insurance, which typically aligns with Medicare requirements.
Who Provides Hospice Services?
Based on an individual’s needs, hospice care is provided by a team of healthcare professionals and volunteers who work to provide comfort to patients who are in the terminal phase of an illness and are no longer seeking life-prolonging treatment. Medicare guidelines require that the team include:
- a registered nurse
- a physician
- a social worker
- a spiritual counselor
- healthcare aides
- trained volunteers
Where is hospice care provided?
While people often believe hospice is a facility, in most instances, it is a service. Hospice is typically provided in the patient’s home, or wherever the patient is most comfortable, such as the home of a family member or friend. Hospice is also provided at:
- skilled nursing facilities
- assisted living facilities
- long-term care facilities
- hospitals
Some communities have dedicated hospice facilities, although this is much less common and varies regionally.
What is the Process of a Hospice referral?
Below are the steps for a typical hospice referral:
Schedule an appointment with your primary care physician to discuss hospice care: The physician will evaluate you to determine if you meet the hospice criteria: a prognosis that there is no hope for their recovery with a life expectancy of six months or less. This includes:
- Reviewing your medical record
- Running tests to further evaluate
- Consulting with any specialists, if necessary, to further evaluate your prognosis.
If the physician is able to determine the patient meets hospice eligibility, the person will receive a referral from the primary care physician to hospice.
Contact Local Hospices. Keep in mind that not all hospices are the same, so be sure to ask questions about the kind of services they provide and make sure they are covered on your insurance. After gathering information from you, the hospice provider normally sets up an appointment designed to:
- Get to know your loved one and what their needs are
- Assess the care needed
- Offer a consultation with other medical personnel who may recommend anything from physical therapy to a specialist if the patient has a decline in their physical or mental well-being.
Review and Accept Hospice Offer: The patient will be required to sign an agreement which states that they understand and accept all terms and conditions for this care, which includes forgoing life-prolonging treatments. If a patient does not want to participate in the program, they have the right to change their mind at any point in time.
How Can I Talk to My Provider about Wanting to initiate Hospice Care?
The following are a few ways you can start the conversation with your provider about hospice care:
- I want to talk with you about how I can maintain control of my life as my illness progresses. I appreciate all you have done to help me fight this disease, but I have come to a place where I want to redirect my remaining energy.
- The quality of my life is important to me and I want to spend my time focusing on the activities that give my life the most meaning.. I believe it is time to talk about a referral to hospice and comfort care only.
- I want my pain to be kept under control, and I want to be kept comfortable until my death.
- I am no longer interested in traditional or experimental procedures designed to prolong my life, I would like to focus on support that helps me to spend time doing the things that matter most to me.
- At this time, I am seeking only one thing: the peace of mind that comes with knowing hospice will be available to me at the time of my choosing.
Does Hospice Shorten the Length of Time a Patient Lives?
No, in fact, evidence-based research and anecdotal experience suggests that hospice can, in some instances, lengthen the time that somebody lives in addition to improving one’s quality of life. As an example, a study in the Journal of Pain and Symptom Management, found that hospice enrollment is not associated with shorter survival rates. Furthermore, some patients with certain terminal diseases who chose hospice lived longer than similar patients who did not receive hospice. This is because hospice helps patients:
- Avoid the risks of over-treatment which can actually reduce both quality of life and length of time lived
- Receive additional monitoring and treatments only available through hospice
- Increase their desire to continue living due to the constant attention to their emotional wellbeing and physical health
How Do I Find and Select a Hospice Care?
Many communities have numerous hospice providers, and you should be able to find one that is aligned with your end-of-life values. It’s important to choose a hospice that is a good fit for your priorities and beliefs, one that will honor your end-of-life care preferences. Some hospices will support you in the full range of end-of-life options such as palliative sedation, voluntarily stopping eating and drinking, and medical aid in dying, while others will not. In addition, services vary by hospice so it’s important to fully understand your options before choosing a hospice.
You can begin learning about different hospices in your community even if you have not yet received a referral:
- Ask friends or family who have had experiences with hospices in your community for advice. A personal recommendation is a good place to begin.
- Ask your referring physician if they prefer a particular hospice and why. This does not mean you have to choose that one.
- Some healthcare systems have policies that could prevent your healthcare providers from supporting you with the full range of end-of-life options (e.g. medical aid in dying, voluntarily stopping eating and drinking (VSED), palliative sedation). If end-of-life options are important to you, ask how the hospice will support you with these options or whether they are governed by any ethical directives that impact the care they will or won’t provide.
- Some insurance companies pay for only a particular hospice. When you contact a hospice, ask whether they take your insurance.
- In addition, you can contact the National Hospice and Palliative Care Organization (NHPCO), which represents most hospice programs in the United States. To find an NHPCO member hospice, call NHPCO’s HelpLine at 1.800.658.8898 or visit NHPCO.org.
Once you’ve found a hospice, call and ask to speak to an intake person. Make sure to take notes. Explain your current medical situation, tell them where you live, and ask questions from the list below that are important to you.
Things to Consider when Selecting a Hospice
Listen for concern, kindness and thoughtful responses.
Patient care
- How will the hospice staff work with me and my loved ones, and honor my wishes?
- How are family caregivers provided the information and training they need to care for me at home?
- How many hours of in-home care will I be provided on a regular basis? What about during a medical crisis?
- What medications that I am currently taking will I no longer be allowed to take?
- Do you have any ethical or religious directives that dictate the care I will or won’t be able to receive?
- Is respite care (relief for the caregiver) readily available?
- Are loved ones told what to expect in the dying process and what happens after I die?
- If I decide to voluntarily stop eating and drinking as I near death, will hospice support me and my family in that process?
- If I live in an authorized state for medical aid in dying, will hospice support me and my family in that process?
- What will happen if care cannot be managed at home?
- What bereavement services are available for my family after I die?
Physician role
- What is the role of my physician once hospice care begins?
- Can I still see my own physician if I want to?
- How will the hospice physician oversee my care and work with my doctor?
Volunteers
- What services do volunteers offer?
Nursing home residents and other residential care settings (if applicable)
- How does the hospice provide services for residents in different care settings?
Comfort and pain management
- Will the hospice staff regularly discuss and routinely evaluate pain control and symptom management with me and my family?
- How quickly does the hospice staff respond to requests for additional pain medication? What is the process for that?
- In the event that the usual doses of oral pain medications are not sufficient to relieve acute distress, is palliative sedation, or total sedation, an option? (Palliative sedation is the medical procedure of intravenous pain medication given to the point of constant deep sleep until death occurs. Some hospices may need to transfer the patient to a healthcare facility in order to provide this service.)
- How will you meet the spiritual and emotional needs of me and my family?
After-hours care
- How quickly does the hospice respond to after-hours emergencies?
- How are calls and visits handled when death occurs?
- What is your weekend and night coverage? (There should be a nurse available by phone 24 hours a day, seven days a week.)
- Are other resources, such as a chaplain or social worker, available after hours?
Paying for hospice care
- Are all of the costs of hospice care covered by my health insurance?
- What services will we have to pay for out of pocket? Are any services provided at no charge?
Making the decision
After you have completed your search, compare the notes you have taken. If you are able, talk with a friend or family member, and seek their input. Do not hesitate to call a hospice back if you need clarification or have lingering questions. These are the people who will play a vital role in the last months and days of your life. You want to feel confident that you will be in good hands and treated competently, respectfully and compassionately.
What happens once I have selected a hospice?
- A nurse and/or social worker will come to your home and complete an intake interview. This visit may last more than an hour. Make sure any friends or family who will be involved in your care are present.
- Take care of yourself. The interview consists of many questions and forms to sign. Depending on how you feel that day, it may be exhausting. If you become too weak or tired to pay attention, ask to have them return the next day. Remember, you are in charge of your care.
- If you have a preference for a male or female nurse, let them know.
- When you meet your nurse for the first time, describe any special needs or concerns you have. Try to let your caregivers know what you want. Do you like to be kept informed? Are you uncomfortable discussing your feelings? Do you have any specific fears about pain or memories of difficult deaths that others have experienced? Are there family issues that are contributing to your stress? The better informed your hospice providers are about your unique concerns, the better able they will be to meet your needs.
- Read through the hospice materials you are given. Make sure everyone involved in your care reads them. Don’t hesitate to ask questions when your nurse visits, or call the hospice in-between visits if questions arise that trouble you.
- You are in charge. If you want the nurse or other members of the hospice team (social workers, spiritual counselors, volunteers or aides) to visit more or less frequently, let them know. If you are uncomfortable with the nurse who has been assigned to you, call the hospice and ask to speak with the nursing supervisor. Explain your concerns and explore whether another nurse can be assigned to your care.
- If you find that the hospice you have chosen is not being responsive to your needs, even though you have brought a matter to their attention, you may always “fire” them and find a new one. (This rarely is necessary, but it is certainly an option to consider.) Check with your insurance provider regarding this possibility.
What happens if a medical crisis develops while in hospice care?
Because you are now a hospice patient, the response to life-threatening situations may differ from what would happen in an earlier stage of your illness. For instance:
- Hospice should be called before calling 911. Make sure anyone staying in the home knows this. Post the hospice number near every phone. Discuss with your hospice nurse what should be done in the event of a medical problem like a fall or a suspected broken bone.
- Hospice will provide you with an out-of-hospital do-not-resuscitate order form (DNR and/or POLST/MOST). If emergency services are accidentally called to your home, this document will inform them that they are not legally bound to perform CPR or resuscitation.
Tools and Resources


