Compassion & Choices is working in states, through the courts and at the federal level to prevent healthcare entities from disregarding patient values and preferences and restricting end-of-life care based on an institution’s ethical and religious policies and directives.
What are Healthcare Facility Refusals to Provide Care?
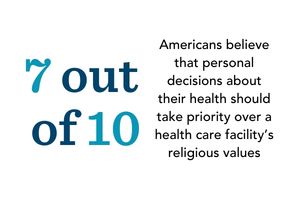
A 2021 study in the Journal of American Medical Association found that an overwhelming 71 percent of Americans believe that personal decisions about their health should take priority over a healthcare facility’s religious values. However, at life’s end, religious institutions often dictate care decisions, regardless of the patient’s preferences.
Healthcare facility refusals to provide care, also known as religious exemptions, religious refusals, denials of care, or “conscience protections'' are policy-based restrictions on healthcare that allow healthcare organizations, doctors, and other healthcare workers to refuse to treat or deny patients access to lawful, medically appropriate care, if it runs counter to their “moral conscience.” In addition to end-of-life care, these restrictions also impact reproductive services and LGBTQ+ care.
Why Is Compassion & Choices Concerned about Health System Refusals to Provide Care?
Unfortunately, at life’s end, many healthcare systems dictate care decisions, regardless of the patient’s preferences, through refusals to provide care and ethical directives. This is particularly true in Catholic health systems, which comprise nearly 80 percent of religious health systems, and whose Ethical and Religious Directives (ERDs) are among the most restrictive and vigorously enforced when it comes to end-of-life care. While many Catholic health systems provide excellent, compassionate care overall, at the end of life, they force patients to endure care inconsistent with, and many times, directly contradictory to, their own values.
Below are some examples:
- If a dying patient’s pain is uncontrollable, under the ethical directives, a doctor is told to help their patients “appreciate the Christian understanding of redemptive suffering.”
- Furthermore, medically-assisted nutrition and hydration must be provided to patients who can reasonably be expected to live indefinitely if given such care. This includes patients suffering from chronic and irreversible conditions, such as a “persistent vegetative state,” when a person is completely unresponsive and being kept alive by medical intervention only.
- In contrast, seven out of 10 Americans believe that end-of-life care should instead prioritize “helping people die without pain, discomfort or stress,” according to a Kaiser Family Foundation survey.
How Big a Problem is This?
- In certain parts of the country, the only hospitals or healthcare facilities serving the public have ethical and religious directives in place that limit or constrain patients’ choice, despite such choices being lawful and medically appropriate options.
- In addition, many hospice entities are also affiliated with hospitals and health systems that have restrictions on end-of-life care services and will deny patients the care they desire, supplanting the desires and religious beliefs of their patients with their own.
- Many physicians who provide end-of-life care are affiliated with a larger medical company; in fact, few physicians are sole proprietors or affiliated with a small practice. Therefore, it is often difficult, if not prohibitive, for patients to find providers not affiliated with an entity that imposes religious beliefs on the patient that they don’t agree with or to find alternate providers.
- Mergers, consolidations and acquisitions of healthcare facilities by religious healthcare entities increase the number of facilities that restrict end-of-life care, impacting all patients, and particularly those who have been historically underserved.
- Unfortunately, the problem is getting worse. In 2020, Community Catalyst published a report, Bigger and Bigger: The Growth of Catholic Health Systems. It noted that the number of Catholic-affiliated hospitals grew by more than 28% over the last two decades, even as the number of secular hospitals dropped by nearly 14%.
Are There Other Reasons Health System Refusals to Provide Care are Problematic?
Healthcare system refusals to provide care are also problematic for the following reasons:
- Transparency is lacking. Religiously-affiliated entities often “hide” their religious affiliation, leaving patients unaware of certain healthcare service restrictions. Without clear, comprehensive information on the full range of end-of-life options and the institution's restrictions, patients are unable to give proper informed consent.
- Individual Patient Freedom is Undermined. Limiting access to certain end-of-life care options undermines individual freedom, particularly given that taxpayer dollars are used to fund care at these institutions. Patients' rights should not be secondary to the rights of institutions.
- Inequities for historically underserved communities are exacerbated. The Community Catalyst report found that in five states (Alaska, Iowa, South Dakota, Washington and Wisconsin) over 40% of all acute care beds are in Catholic hospitals. Fifty-two hospitals are designated as the sole community hospital (at least 35 miles away from another hospital) in their region. That means many people residing in rural areas, for example, may not have any other options for care.
- Clinician-patient trust is eroded. Health care system refusals to provide care for individuals leave providers unable to provide patients with the care they want at life’s end. Mistrust and denied care hinder clinician-patient recommendations for palliative care or hospice, resulting in more aggressive and futile treatment at the end of life.
But Shouldn’t Providers Be Allowed to Opt-Out of Medical Care They Object to?
We do agree that individual providers should have the right to opt out of participating in end-of-life healthcare treatments they object to based on conscience or religious grounds; however, providers took an oath to care and treat. People have the right to compassionate, respectful and timely end-of-life care and the freedom to make their own healthcare decisions. Providers should not be allowed to use a religious exemption to abandon patients, mislead them, discriminate, or block their preferred care. Providers still have a legal and moral obligation to:
- fully inform their patients of all end-of-life options
- document their requests in their medical record, and
- refer them to another healthcare professional.
What’s an Example of Attempts to Expand Refusals to Provide Care?
A federal rule issued in 2019 by the "Conscience and Religious Freedom" division of the U.S. Department of Health and Human Services Office for Civil Rights attempted to tip the scales to allow religious doctrine — not patient values — to dictate patient care.
This final "conscience rule" allowed any individual or entity involved in a patient's care — from a hospital's board of directors to the receptionist who schedules procedures — to put their personal beliefs ahead of a patient's health and values without any duty to make sure somebody else treats them. The rule increased funding for enforcement and hospitals that didn't follow this directive would have lost their federal funding for patient services.
If implemented, the rule would have significantly and unjustly harmed patients by:
- Creating fundamental barriers to their ability to seek many legal end-of-life care options, such as voluntarily stopping eating and drinking; palliative sedation and even the withdrawal of life-sustaining treatment.
- Creating additional anxiety among vulnerable individuals who now have to worry whether medical providers will refuse to honor their healthcare decisions.
- Expanding the definition of “referral” to include providing information. This means doctors could even object to transferring a patient’s medical record, leaving the patient without the ability to secure another doctor to carry out their preferences.
- Allowing federal fax dollars to be used to protect the physicians who willfully mislead and abandon patients.
Fortunately, 23 Attorney Generals and city counsels across the country immediately litigated the constitutionality of the rule and the rule was vacated. Compassion & Choices is seeking to rescind the rule permanently.
Other examples include opposition-filed lawsuits in New Jersey and California arguing that the state’s medical aid in dying laws are unconstitutional. While the laws include provisions that allow doctors to opt-out of participating in medical aid in dying, the lawsuits claim that a doctor's obligation to transfer the medical record or document a patient’s request for medical aid in dying is a violation of their 1st Amendment rights. The opposition claim directly contradicts the long-practiced standard of medical care, which is based on a doctor’s oath to their patients and an understanding that patients, not doctors, own their medical records.
What Can be Done to Limit the Negative Impact of Health Care Facility Refusals to Provide Care?
On a personal level, patients should interview their health facilities and care providers to determine whether ethical and religious directives or other policy-based restrictions govern their treatment plans and consider transferring care to another provider if the answer is concerning.
On a more global level, we are employing an integrated approach to combat healthcare facility refusals to provide care, which includes:
- Creating and supporting legislation that allows physicians to opt-out without blocking care. We are actively monitoring and pursuing legislation that continues to give doctors and other healthcare providers the ability to opt-out of prescribing aid-in-dying medication without allowing them to impose their values in a way that would block care.
- Developing innovative ways to ensure patients get complete information. The old adage, knowledge is power, has never been more apt than with healthcare. We must look for ways to ensure patients get clear and honest information about the full spectrum of end-of-life options to make informed decisions about where and what type of treatment they want to receive (think cigarette warning labels).
- Protecting the right of patients to information transparency in regulatory rules and court cases. In collaboration with others, we will engage in litigation, legislation and regulatory action to prevent providers from: withholding vital information from patients about their treatment options, deliberately disregarding patient instructions about their end-of-life care preferences or blocking patient access to end-of-life care services.
- Encouraging adoption of patient-directed care policies. At the community level, we continue our successful efforts to convince as many health systems as possible to adopt supportive policies. Using the power of grassroots organizing and public comment to convince as many health systems and hospices as possible to adopt policies supportive of patient-directed care.
- Opposing consolidations and mergers of institutions that arbitrarily limit lawful options regardless of the patient’s values and religious beliefs. As resources permit, we will join with others to actively and vigorously oppose mergers between secular and religiously-affiliated healthcare systems, especially if the merger will leave a community with no other option.
- Expanding education to physicians and pharmacists. We will continue our education efforts to reach clinicians and pharmacists about the importance of practicing patient-directed end-of-life care, helping providers to recognize the importance of respecting and honoring their patients' own beliefs.
Op-Eds by Kim Callinan
- Part I: Growth of Religiously-Affiliated Healthcare Institutions: Why it Matters
- Part II: Growth of Religiously-Affiliated Healthcare Institutions: Our Path Forward
- Medical Emergency: The Chart State Wall Has Collapsed
- Immediate Actions the New Administration Should Take to Improve Advance Care Planning
- New Federal Rule Puts Patients' Rights at Risk
- Religious Freedom at Life’s End: An Aspiration that’s Worth the Fight
- Hospital Merger Imperils Options for End-of-Life Care


