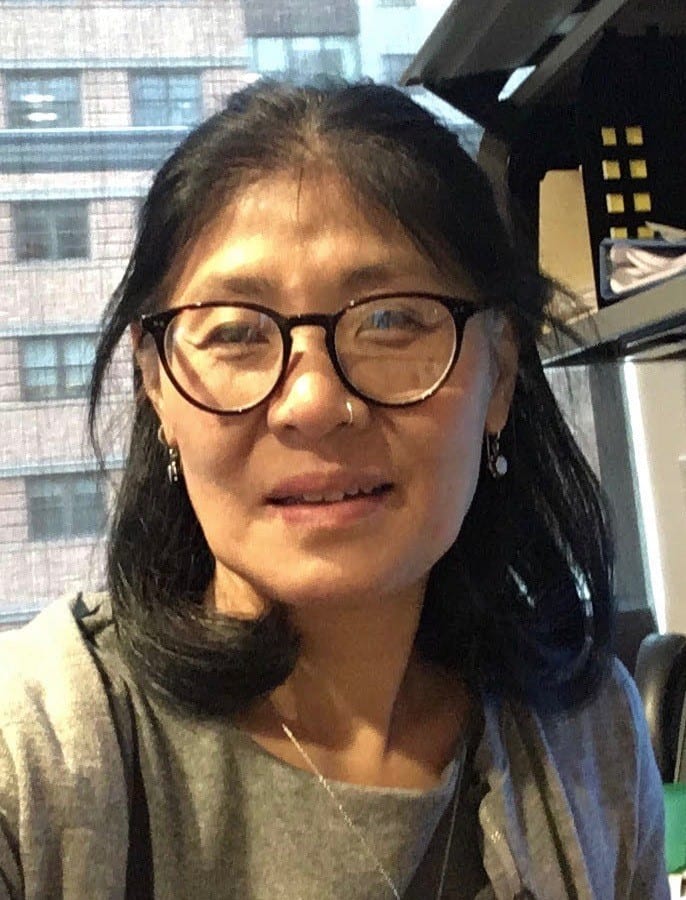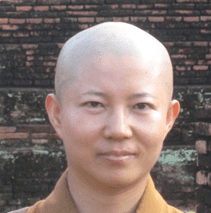
Venerable Zhiyun Cai, PhD, BCC, PCHAC, AIHCP Certified Grief Counselor, Palliative Care Chaplain, Stanford University Hospital
Bhikkhuni Dr. Zhiyun Cai is a palliative care chaplain at Stanford Hospital, a scholar and a practitioner. She holds a Ph.D. in Religious Studies. She is also the first Buddhist foreigner to earn the certification of the Board Certificated Chaplain (BCC) through the Association of Professional Chaplains in the United States.
Bhikkhuni Dr. Zhiyun ordained as a Buddhist nun in the Zen Buddhist tradition in 1993 in China. She had received three primary Buddhist schools’ training (Theravada Buddhism, Mahayana Buddhism, and Vajrayana Buddhism) in her early monastic life. She was invited to the United States in 2000 by a Buddhist organization. She was impressed by the extensive mindfulness practice of westerners. She conducted researches and completed her dissertation on “Doctrinal Analysis of the Origin and Evolution of the Buddhist Forest Meditation Tradition with a Special Reference to the Thai Present Forest Ajahns.” This is the first research to discuss the similarities and the differences between the Buddhist original forest meditation teachings from the Pāli Canon and the modern meditation techniques that are widely applied in the United States. The research provides rich content on the meditation both to scholars and practitioners.
Bhikkhuni Dr. Zhiyun received her interfaith Chaplaincy Resident and Palliative Care specialty training at Stanford Health Care. She provides compassionate, professional, and effective spiritual care services to patients with serious illness for more than ten years. She has rich experience in palliative and hospice spiritual care. Bhikkhuni Dr. Zhiyun also offers mindfulness and self-compassion courses to the hospital staff and local university students to increase their resilience for living a better life. She is involved in training new interfaith chaplain at the hospital, works with local Buddhist communities, hospital palliative medicine teams to increase patients’ quality of life, valued their end of life decision, assist them with a dignified and peaceful death. Bhikkhuni Dr. Zhiyun traveled extensively in the United States and overseas to provide spiritual care, retreat, and assist the Buddhist communities in establishing Buddhist Compassionate Care Center to patients with life-threatening diseases. She serves in the Wellness Committee at Stanford Health Care. Her clinical research focus on mindfulness training for increasing the quality of life of the Palliative Care patients, Self-Calming Rituals, Competency Cultural Education, and Asian Perceptive on Death and Dying. Chaplain Yun recently earned the Palliative Care and Hospice Advanced Certification (PCHAC)from APC and became one of only forty-four such certification holders in the United States.


.jpg?sfvrsn=d12a7036_3)